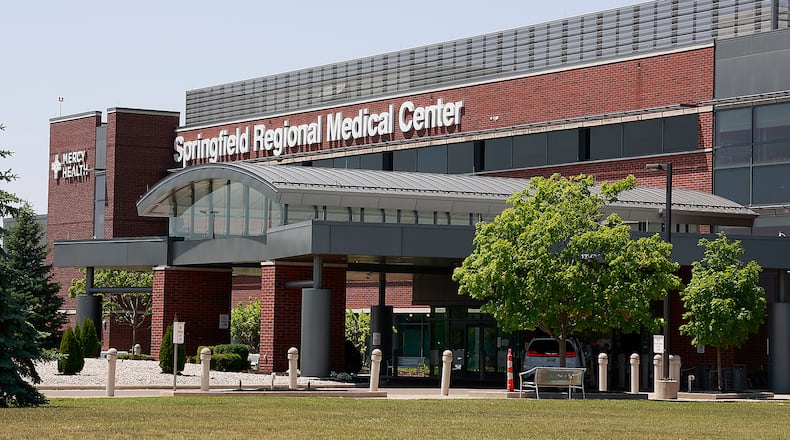
“We understand that being out network can be very difficult, and we are pleased that patients with Anthem insurance can now see our physicians and use our hospitals at an in-network cost,” said Adam Groshans, president of the Mercy Health – Springfield market. “We sincerely believe that access to quality health care services is vital for our communities. This new agreement protects our patients’ access to compassionate care close to home.”
Mercy Health has hospital and medical office locations in Butler, Clark, Greene and Hamilton counties in this region.
Anthem has agreed to cover any claims that patients may have incurred during the period of time that Mercy Health was out-of-network with Anthem Medicaid since July 1. The agreement also extends coverage for Anthem employer-based and Affordable Care Act plans. This new agreement between Mercy Health and Anthem is also extended until 2028.
This agreement follows months of uncertainty for Anthem Medicaid members as the insurance provider and hospital network debated undisclosed pricing. Hospitals have faced increased costs, a Mercy Health spokesperson said, while Anthem said the requested cost increases for its employer-sponsored and Affordable Care Act plans was too high.
The Ohio Department of Medicaid also previously rejected a request from Mercy Health to freeze enrollment in Anthem’s Medicaid managed care plans and transfer members to new Medicaid plans if they were an active Mercy Health patient.
“I’m proud that both organizations continued to focus on our shared priority: the communities we serve,” said Jane Peterson, Anthem Ohio president. “We worked together to creatively address affordability for our members and the financial needs of an important care provider. This agreement provides long-term stable access to care at Mercy Health without cost increases for our members and employers.”
Details of the agreement are not being released due to confidentiality provisions in the contract, Mercy Health and Anthem both said.
As part of the agreement, Mercy Health has agreed to dismiss the Virginia lawsuit, saying the organizations will form teams to address claims submissions and payment processes. The lawsuit had previously alleged Anthem had $93 million in unpaid claims to Mercy Health in Virginia, which Anthem disputed.
Mercy Health’s parent company, Bon Secours Mercy Health, is the fifth largest Catholic hospital system in the U.S., with 47 hospitals, 3,000 physicians and 60,000 associates across seven states and Ireland.
The 2022 operating revenue for Elevance Health, the parent company of Anthem, grew 13.7% year-over-year to $156 billion, with its 2022 operating gain growing 12.9% year-over-year to $8.5 billion, according to its earnings report. Bon Secours Mercy Health reported an overall loss of $1.2 billion in 2022, the hospital system said.
Anthem members may contact the Member Service phone number on their Anthem ID card for assistance with any questions. Mercy Health patients may also call 888-354-0205 for more information.
About the Author