Physicians at Dayton-area hospitals have also observed similar patterns.
Dr. Jeffrey Weinstein, the patient safety officer and a medical doctor at Kettering Health, said the data shows how rare it is to get COVID-19 after being fully vaccinated, meaning two weeks after the second shot of Moderna or Pfizer vaccines, or two weeks after a Johnson & Johnson vaccine.
“Most of our patients being admitted over the last couple of months, with COVID-19 infection, have been unvaccinated,” he said. “And we’ve had some who were partially vaccinated but not fully vaccinated. Among our staff, it’s the same.”
A spokesman for Premier Health said the health system had seen a similar trend to the Cleveland Clinic’s data at its hospitals.
“This data reinforces the efficacy data that has been so prevalent in our public health messaging,” said Dr. Roberto Colón, chief medical officer at Miami Valley Hospital. “These vaccines do work, and they help lower the severity of illness in the very rare cases of breakthrough infections.”
As of Tuesday, about 45% of Ohioans had started at least one dose of the COVID-19 vaccine, according to the Ohio Department of Public Health. In Montgomery County, about 43% of the population had gotten at least one dose of the vaccine, and in Greene County, about 44% of the population had at least one dose, though Wright-Patterson Air Force Base has a separate vaccination system.
Weinstein said with a disease like COVID-19, which is so easily spread, and a high population of people who have gotten the vaccine, it’s easier to measure effectiveness. The vaccine is very effective, he noted.
“The more effective that vaccine is, the less hesitant people should be, or we would hope that they would be,” he said.
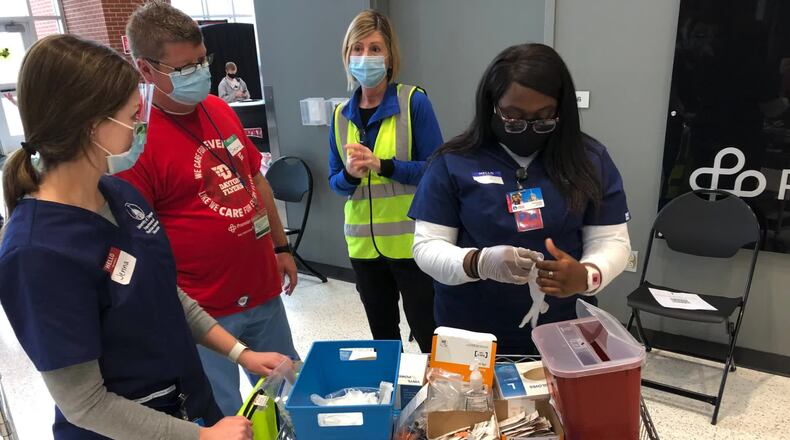
Sarah Hackenbracht, president and CEO of the Greater Dayton Area Hospital Association, said hospitals, public health officials and the community are still working together to make sure the COVID-19 vaccine is widely available.
Instead of having individual mass vaccination sites, she said, they’re working to get vaccines to be available at a local barber shop, in community events or at a mobile vaccine clinic.
In some counties, Hackenbracht noted there are addition incentives, like giving out ice cream at a local ice cream shop after a vaccine.
“It helps really that individual as well because this is still a new and novel diagnosis and we know that some people are having longer term effects of COVID-19, and I don’t think anyone wants that,” Hackenbracht said.
About the Author