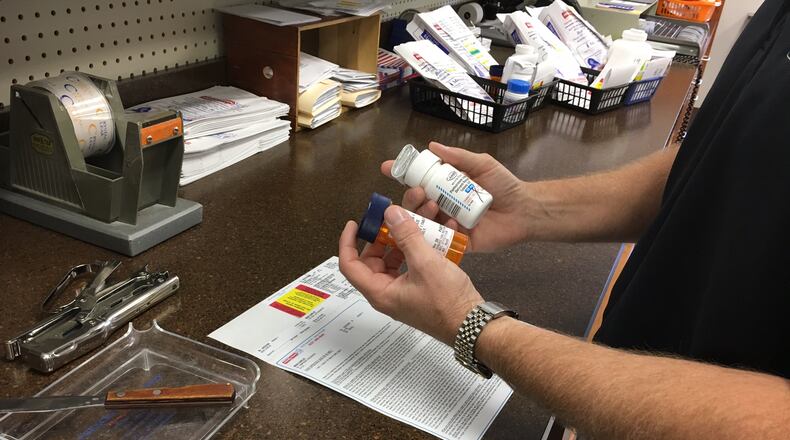
The health system said this means they can share prescription benefit information with patients, including:
· Accurate out-of-pocket medication cost,
· Appropriate medication alternatives,
· And pricing at multiple pharmacies.
“We will be one of the first health networks in the country to offer the newest version of this unique tool that provides full drug cost transparency to patients at the time of prescribing. The ultimate goal is to improve patient access to needed medications,” Jim O’Donnell executive director of Pharmacy Services at Kettering Health Network, said in a statement about the program, CenterX.
CenterX Real-Time Pharmacy Benefit and Electronic Prior Authorization are integrated within a health system’s electronic health records to provide complete, patient-specific benefits data and a prior authorization.
The company said it helps “reduce cost and increase revenue, improving medication adherence for every patient, every time.”
Kettering Health operates Fort Hamilton, Grandview, Greene Memorial, Kettering Behavioral Medicine Center, Kettering, Soin, Southview, Sycamore, and Troy hospitals. They also operate a network of primary and specialty practices, outpatient sites and free standing emergency centers.
Antonio Ciaccia, Chief Strategy Office at 3 Axis Advisors, which consults on pharmacy issues, said the fine details of a program are important, such as whether there are any biases in a system that could steer where patients go, but the idea of getting the patient real cost information means equipping them to be better advocates for themselves.
“If it’s as good as it sounds, on the surface, I think that’s an incredible weapon. Because half the battle is getting your prescriber to be sensitive to the price as well. And the patient is traditionally very underequipped to even push back,” Ciaccia said. “You go to your pharmacy, and then you find out.”
He said real cost information could also prevent a billing surprise when filling a prescription, which can have health and financial consequences.
“One big issue is that when patients get that sticker shock at a pharmacy, what often occurs is they say, ‘I can’t afford that.’ And they’ll either only get a portion of it or they’ll just forego the prescription altogether,” Ciaccia said.
About the Author