“I am extremely proud of our medics!” said Col. Shari Silverman, 88 MDG commander. “The Joint Commission survey just validated what my family and I already knew, that our facility delivers high-quality, Trusted Care every day. We are proud to serve our nation’s veterans and families.”
According to The Joint Commission, the survey process is data-driven, patient-centered and focused on evaluating actual care processes. On-site surveys are designed to be organization-specific, consistent and supportive of the organization’s efforts to improve performance.
About 21,000 health care organizations and programs in the U.S. are accredited and certified by The Joint Commission. Accreditation and certification is recognized nationwide as a symbol of quality that reflects an organization’s commitment to meet certain performance standards.
“The Joint Commission is a civilian accredited agency that reviews military treatment facilities every three years,” said Capt. Christina Nigro, Organizational Improvement Office inspection compliance manager. “Although the survey is every three years, we still conduct thorough self-assessments of all the elements of performances during the survey off-years. Similar to a Unit Effectiveness Inspection, the survey ensures that we are complying with their standards.”
The team of surveyors looked at 267 standards and within those standards, there are 1,544 elements of performance.
The elements of performance that are looked at by The Joint Commission team encompasses a head-to-toe review of the medical center and reviews all aspects of patient safety and care. Elements of performance range from proper egress and patient identification to correct handwashing procedures.
Some methodology used during the survey process include tracer methodology for assessing standards compliance. Individual tracers begin at the point of care of an individual patient and provides a roadmap to move through the organization to assess and evaluate the care, treatment and services received by the patient. System tracers follow one system across the organization’s continuum of care and look at data management, infection control, medication management, credentialing and privileging, environment of care, emergency management and competency.
To receive certification in Primary Care Medical Home, the medical center complied in an additional 46 elements of performance in pediatrics, family health, internal medicine and flight medicine. Currently, only 33 percent of hospitals in the Air Force are Primary Care Medical Home certified.
“Our goal is to make sure that whoever comes into this facility, whether they are a patient or staff member, can feel comfortable that their safety is considered and that it is our prime focus,” said Gerry Laughner, director of the Organizational Improvement Office.
Laughner said their safety incident record for a medical center who sees an average of 1,200 outpatients per day and 24 inpatients is remarkable. As of June 14, it has been 510 days since the last serious patient safety event.
In the event of a mishap, the Organizational Improvement Office maintains a database to track and reviews patient safety incidents. Tracking the incidents help find ways to improve as well as monitor for any potential trends.
Laughner credits the Trusted Care Program for a large part of their success with patient safety.
Trusted Care is a program that works on continually improving the culture of safety and reliability within the Air Force Medical Service. Four domains, comprising leadership engagement, culture of safety, continuous process improvement and patient centeredness has been adopted to reflect the commitment of placing patients first.
Daily “huddles” with leadership to discuss safety concerns, training all staff members in Trusted Care and recognizing staff members as “Trusted Care Heroes” when going above and beyond to identify safety concerns are some of the ongoing practices of the medical center.
Laughner said empowering staff members to engage in identifying safety concerns and suggesting solutions is key to the Trusted Care Program.
“We highly encourage staff members to help with process improvements,” said Laughner. “Everyone’s desktop has an icon of a program where employees can report safety incidents.
“In addition, when staff members engage, it enables our office to have more accurate information to track trends or other safety concerns. We may find that if it is happening in one clinic, it could be happening in another.”
Another program encouraging input from all staff members is Lean Daily Management. There are currently 60 LDM boards maintained in numerous sections within the medical group which are targeted to improve a current process for that area. Staff members work together to figure out what the root cause is and try to find solutions to make the process smoother, quicker or safer.
Five days a week, medical center leadership make rounds to the clinics to review the suggested improvements for possible implementation of the proposals.
“We take patient safety and zero harm very seriously,” said Laughner. “We are happy to provide the safety care that we do; it is not a burden. It is work but well worth it. The entire medical group staff are champions of patient safety; we want to get to zero harm and we believe we can do it.”
During The Joint Commission survey, surveyors noted five best practices and two leading practices in the following areas:
Best practices
- Mental Health/Neuropsychology Program
- Mental Health/Inside Out Program
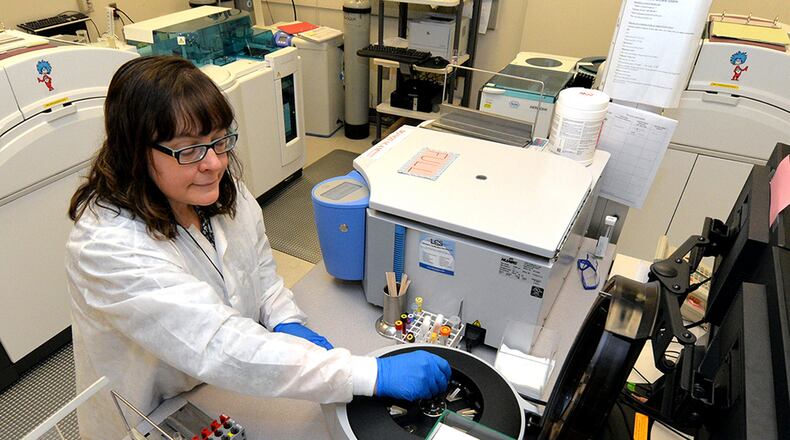
- Emergency Department/Blood Collection System
- Emergency Management/Exercise Management
- Dental Instrument Processing Center
Leading practices
- Education and Training/Nurse Peer Review
- Specimen Collection Dermatology/Specimen Chain of Custody
In addition, nine individuals were recognized as star performers:
- Maj. Gary Leavitt, Operating Room
- Maj. Saul Freedman, Mental Health
- Maj. David Lindholm, Antimicrobial Stewardship Program
- Capt. Ladylaarni Domingo, Intensive Care Unit
- 1st Lt. Matthew Jacobson, Dialysis
- Staff Sgt. Jonathon Buchanan, Dental Clinic
- Senior Airman Daniel Acchione, Dental Clinic
- Vincent Robertson, Dental Clinic
- Andy Shirey, Facilities and Team
About the Author